
By:
- Scott LaFee
Published Date
By:
- Scott LaFee
Share This:
HIV Prevention in a Pill
UC San Diego researchers receive $5.6 million grant to test if they can keep high-risk individuals from becoming infected with virus that causes AIDS
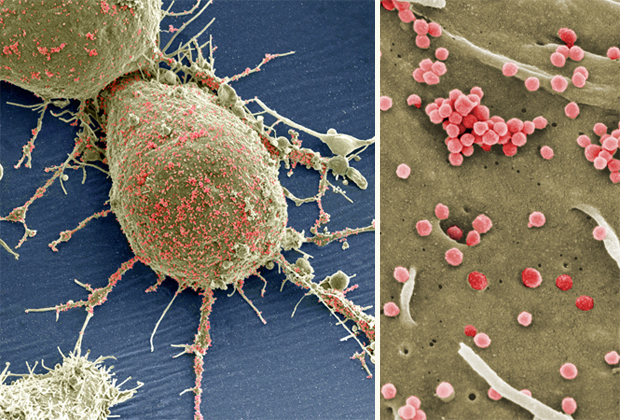
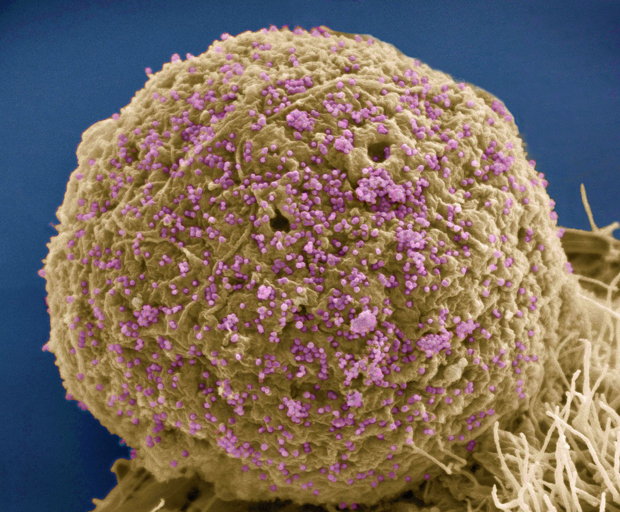
In these scanning electron micrographs from Thomas Deerinck at the National Center for Microscopy and Imaging Research at UC San Diego, multitudinous HIV-1 particles exit from a cultured HeLa cell. The image is false-colored.
Last year marked the 30th anniversary of the first clinical reports of AIDS, a then-mysterious and invariably fatal disease. Patients diagnosed with an HIV infection faced a looming death sentence. Most had just months to live.
“It was hugely disheartening,” recalls Dr. Douglas Richman, a professor in the departments of pathology and medicine at UC San Diego and longtime AIDS researcher. “We felt like battlefield doctors with the sick and dying coming in faster than we could treat them – if we could treat them at all.”
Much has changed, of course. These days, scientists and physicians like Richman better understand the pathology of HIV/AIDS and the advent of antiretroviral drugs (prescribed in the early stages of infection) can often render HIV/AIDS a chronic but livable condition. Patients can live relatively normal, full lives for decades after diagnosis.
Perhaps the greater challenge now is preventing HIV infection in the first place, particularly among persons at high risk, such as men who have sex with men and transgender women. In the largest test of its kind, researchers at UC San Diego and two other UC campuses will try to do just that, testing a potential HIV prevention pill, along with new strategies to keep HIV-infected persons in care and treatment.
“Despite the message for now almost 30 years of using condoms and being faithful, HIV is still being transmitted,” said Dr. Richard Haubrich, a professor in the UC San Diego School of Medicine and Antiviral Research Center, in a recent interview with KPBS. “Because of that, I think newer strategies, for some people, not for everybody, should be looked at.”
Haubrich will head the UC San Diego component of a new $11.8 million project funded by the California HIV/AIDS Research Program, part of the UC Office of the President. With colleagues, Haubrich will enroll 400 study HIV-uninfected gay men and transgender women (male to female) living in San Diego, Los Angeles and Long Beach. Each enrollee will receive a daily pill that combines two antiretroviral drugs (tenofovir and emtricitabine), marketed as Truvada by its maker Gilead Sciences, Inc.
“Truvada is one of the most used medications for treating HIV,” said Haubrich. “We know a lot about it and how it works. It lasts a long time in the body. It’s very safe and a number of randomized clinical studies have shown that it reduces risk of infection. It’s this combination of things that prompts us to use it to try to prevent infections.”
The antiretroviral pill is part of a larger intervention effort called “Pre-Exposure Prophylaxis with antiretroviral drugs” or PrEP. The researchers will also develop and study ways to help identify, engage and retain HIV-infected persons in interventional treatment programs. Among them: Sending out daily, self-designed text messages to remind participants to take their medicine.
“It’s no surprise to know that if you don’t take a medicine, it’s not going to work,” Haubrich said. “But erratic use can be little or no better than not taking a medicine at all. This study is too small to prove the efficacy of the pill, but if we can show in a clinical setting that people can take the medicine on a regular basis, that will be a big plus.”
The UC San Diego-based program will receive $5.6 million in funding and will run for four years. The other two, related efforts are based at UCLA and UC San Francisco.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.


