
HIV Infection Prematurely Ages People by an Average of Five Years
Epigenetic changes also associated with 19 percent increased risk of mortality
Published Date
By:
- Heather Buschman, PhD
Share This:
Article Content
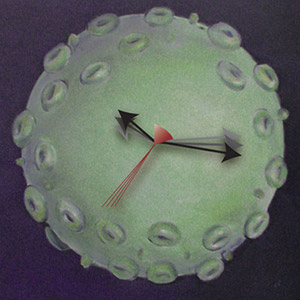
The epigenome provides a good measure of aging, serving as a biological clock. Epigenetic age is increased in antiretroviral-treated, HIV-infected individuals, represented here by a rendering of the viral surface and advancement of clock hands. Design by Robin Taylor, HIV artwork by Emily Harrison.
Thanks to combination antiretroviral therapies, many people with HIV can expect to live decades after being infected. Yet doctors have observed these patients often show signs of premature aging. Researchers at University of California San Diego School of Medicine and the University of Nebraska Medical Center have applied a highly accurate biomarker to measure just how much HIV infection ages people at the cellular level — an average of almost five years.
The study is published April 21 in Molecular Cell.
“The medical issues in treating people with HIV have changed,” said Howard Fox, MD, PhD, professor at the University of Nebraska Medical Center and one of the authors of the new study. “We’re no longer as worried about infections that come from being immunocompromised. Now we worry about diseases related to aging, like cardiovascular disease, neurocognitive impairment and liver problems.”
The tool used in the new study looks at epigenetic changes in people’s cells. Epigenetic changes affect DNA structure, but not DNA sequence. Once epigenetic changes occur, they are passed down from one generation of cell to the next, influencing how genes are expressed. The particular epigenetic change used as a biomarker in this research was methylation, the process by which small chemical groups are attached to DNA. Methylation of DNA can impact how genes get translated into proteins.
“What we’ve seen in previous studies is that as we age, methylation across the entire genome changes,” said co-corresponding author Trey Ideker, PhD, professor of genetics in UC San Diego School of Medicine. “Some people call it entropy or genetic drift. Although we’re not sure of the exact mechanism by which these epigenetic changes lead to symptoms of aging, it’s a trend that we can measure inside people’s cells.”
The 137 patients included in the analysis were enrolled in CHARTER (the CNS Antiretroviral Therapy Effects Research study), a long-term study to monitor HIV-infected individuals who are being treated with combination antiretroviral therapy. Subjects who were chosen didn’t have other health conditions that could skew the results. Forty-four HIV-negative control subjects were also included in the initial analysis. An independent group of 48 subjects, both HIV positive and negative, was used to confirm the findings.
In addition to the discovery that HIV infection led to an average advance in biological aging of 4.9 years, the researchers note that such a change correlates with an increased risk of mortality of 19 percent.
“We set out to look at the effects of HIV infection on methylation, and I was surprised that we found such a strong aging effect,” Ideker said.
“Another thing that was surprising was that there was no difference between the methylation patterns in those people who were recently infected (less than five years) and those with chronic infection (more than 12 years),” Fox added.
The researchers say it’s possible drugs could eventually be developed to target the kinds of epigenetic changes observed in the study. But the more immediate implications are much simpler: they note that people infected with HIV should be aware that they are at greater risk for age-related diseases and work to diminish those risks by making healthy lifestyle choices regarding exercise, diet, and drug, alcohol and tobacco use.
Study co-authors include Andrew M. Gross, Philipp A. Jaeger, Jason F. Kreisberg, Katherine Licon, Kristen L. Jepsen, Mahdieh Khosroheidari, Ken Flagg, Daniel Chen, UC San Diego; Brenda M. Morsey, University of Nebraska Medical Center; Hui Shen, Van Andel Research Institute; and Kang Zhang, UC San Diego and Veterans Affairs San Diego Healthcare System.
This research was funded, in part, by the National Institutes of Health (grants U24CA184427; P30MH062261, P30CA023100 and HHSN271201000030C) and the California Institute for Regenerative Medicine.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.


