Acting Student and Bioengineering Alumna Awarded Soros Fellowship for New Americans
Awards & Accolades
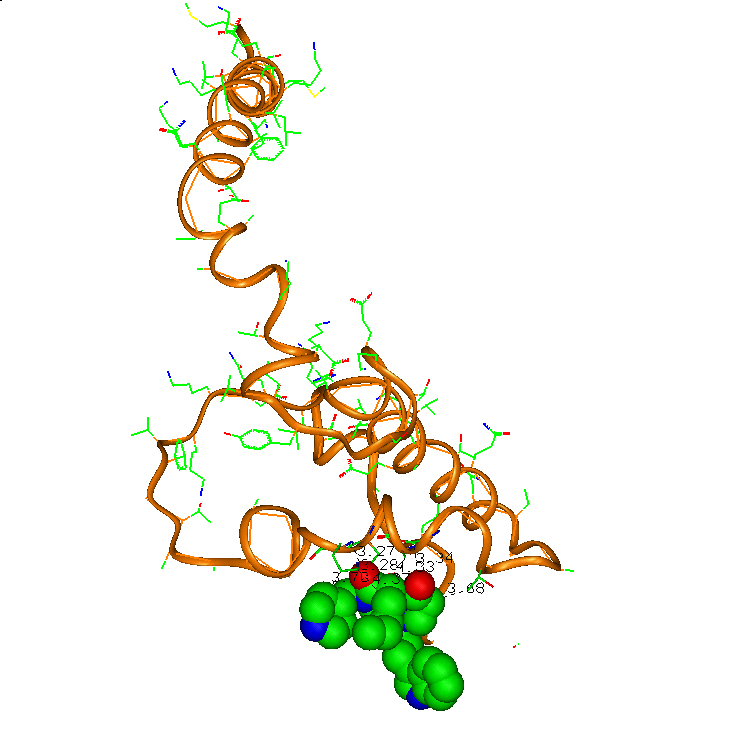
Interaction of the compound (colored by atoms: green-carbon, red-oxygen, blue-nitrogen) with alpha-synuclein (brown ribbon with color by atoms side chains). Igor Tsigelny, UC San Diego
An international team led by University of California San Diego researchers has employed a novel computational approach to design and create a new compound that in laboratory studies has reduced deficits and neurodegenerative symptoms that underlie Parkinson’s disease.
In a study published in the September 27 Advance Access issue of Brain, the researchers describe how their compound, dubbed NPT100-18A, prevents the binding and accumulation of alpha-synuclein or α-syn in neuronal membranes, now considered a hallmark of Parkinson’s disease and a related disorder called dementia with Lewy bodies.
“We’ve demonstrated a novel computational approach to design potential therapies for Parkinson’s disease and related disorders,” said the study’s co-first author Igor Tsigelny, a research scientist with the San Diego Supercomputer Center (SDSC) at UC San Diego, as well as the UC San Diego Moores Cancer Center and Department of Neurosciences.
Added Eliezer Masliah, the study’s principal investigator and former professor in UC San Diego School of Medicine’s Department of Neurosciences: “It’s a first step, but we believe it’s a big step.”
Parkinson’s disease, which affects more than 10 million people worldwide, is characterized by impairment or deterioration of neurons in the area of the brain known as the substantia nigra. The disease typically occurs in people over the age of 60, with symptoms of shaking, rigidity, difficulty in walking, generally developing slowly over time and sometimes followed later by impairment in behavior and thought processes.
Since most symptoms of Parkinson’s disease are triggered by a lack of dopamine in the brain, many medications are aimed at either temporarily replenishing dopamine or mimicking the action of this brain chemical. Unfortunately, current drugs have only a limited impact on long-term neurological deficits and mortality.
For this reason, scientists have begun to focus their efforts on α-syn’s role in the disease, based largely on computer modeling describing how mutant forms of this protein penetrate and coil in cell membranes, and then aggregate in a matter of nanoseconds into dangerous ring structures that open pores to toxic ions that ultimately destroy neurons. The modeling has been supported by electron microscopy showing how damaged neurons in Parkinson’s patients are riddled with these ring structures.
Following this discovery in 2012, UC San Diego researchers began an intense search to identify drug candidates that could block the early formation of ring structures. Specifically, the researchers homed in on “hot spots” that block the binding of two α-syn proteins, or dimers.
But the hunt proved highly complex, owing largely to the nature of the unstructured state of α-syn, sometimes referred to as a “chameleon” that constantly shifts its shape, somewhat like a slinky that’s bobbing and weaving on top of an earthquake epicenter.
“Our biggest hurdle was that α-syn doesn’t have any stable conformation,” said Tsigelny. “So long simulations were needed to define a huge set of possible conformations to find clusters of possible compounds that would work.”
Enter several supercomputers – including Trestles, Gordon, and the Triton Shared Computing Cluster, all based at SDSC; and Blue Gene, with the Argonne National Laboratory – that performed molecular dynamic simulations of in silico structures that would displace α-syn from cell membranes.
“Essentially, this compound mimics the protein’s amino acids in the place where two α-synucleins come into contact, thus preventing the binding of the second protein,” said Wrasidlo, previously with UC San Diego Moores Cancer Center, and the study’s first author.
Subsequent electron microscopy imaging by researchers at the University of Vienna demonstrated that the new compound reduced the formation of α-syn clusters in cell membranes. Further studies with “transgenic” mouse models prone to Parkinson’s disease, both at UC San Diego and UCLA, concluded that the compound improved behavioral deficits and neurodegeneration. Within an hour after it was administered, imaging studies in these mice further showed that the compound reduced accumulation of α-syn in cortical synapses.
“Specifically targeting the α-synuclein structure that is stabilized in cell membranes also allows for a more specific molecularly targeted drug design,” added Masliah.
Though highly encouraging, the researchers caution that the compound needs to be refined before clinical trials can be launched in the future.
Also contributing to the study, titled “A De Novo Compound Targeting Alpha-Synuclein Improves Deficits in Models of Parkinson’s Disease,” were Edward Rockenstein, Simona Eleuteri, Valentina Kouznetsova, Brian Spencer, Paula Desplats, Tania Gonzalez-Ruelas, Margaritha Trejo, and Cassia Overk, all from UC San Diego; Garima Dutta, Chunni Zhu, and Marie-Francoise, all from UCLA; Thomas Schwartz, Karin Ledolter and Robert Konrat, all from the University of Vienna; Diana Price, Douglas Bonhaus, Amy Paulino and Dieter Meier, all from Neuropore, based in San Diego; Stefan Winter and Herbert Moessler, from EVER Neuropharma, based in Austria; and Age Skjevik, from the University of Bergen in Norway.
Funding for the research came from NIH grant AG18440, The Michael J. Fox Foundation for Parkinson’s Research, and Neuropore Therapies.
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.