
UC San Diego Researchers Receive $3 Million Grant from California Stem Cell Agency
The team is developing a treatment for peripheral artery disease
Published Date
By:
- Ioana Patringenaru
Share This:
Article Content
Researchers at UC San Diego received more than $3 million to develop a hydrogel to help people with peripheral arterial disease.
Researchers led by Karen Christman, a bioengineering professor at the University of California San Diego, were awarded nearly $3.1 million by the governing Board of the California Institute for Regenerative Medicine March 23.
Their work aims to help people with peripheral arterial disease. The condition narrows and blocks arteries providing blood supply to the legs resulting in cramping, pain and fatigue condition called critical limb ischemia. It leads to an estimated 230,000 amputations every year in North America and Europe. The new therapy could prevent or limit amputations for a condition that affects more than 27 million people worldwide.
“Taking a promising therapy and moving it out of the lab and into clinical trials takes a lot of expertise and money,” says C. Randal Mills, President and CEO of CIRM. “Our Translational program provides both, giving scientists the support they need to complete the research and get approval to start a clinical trial where we see if this work can really help people in need.”
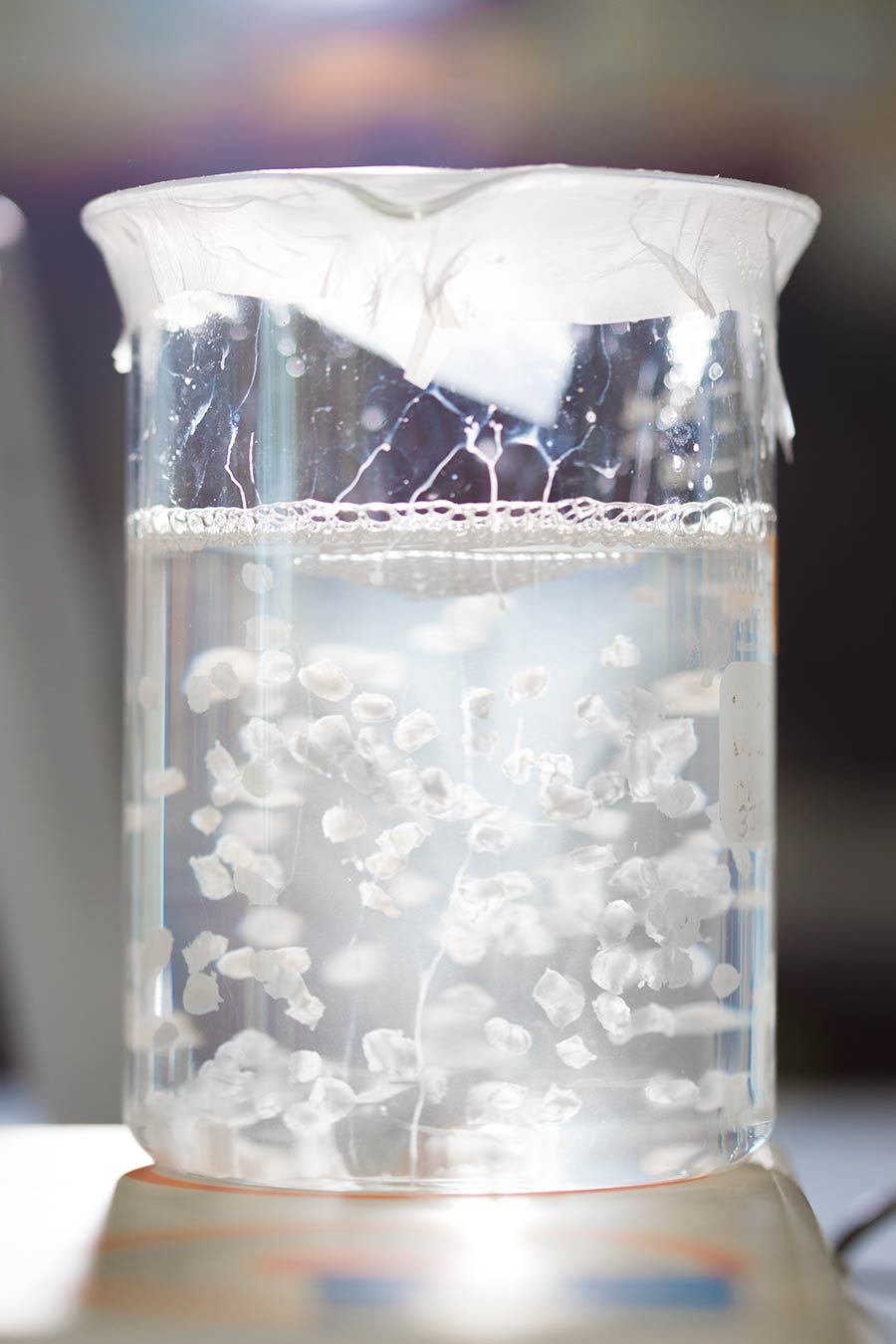
The UC San Diego team has developed a hydrogel that can be injected into the muscles in the leg, creating an acellular scaffold that can result in new blood vessel formation to improve blood flow, and also help stimulate muscle regeneration. The team hopes that this will result in improved walking capacity and increased quality of life for peripheral arterial disease patients. It also has the potential to limit amputations by helping wound healing in critical limb ischemia patients. Last year, the team tested the procedure in a rat model of the disease and found that it promotes muscle remodeling and improves blood flow.
“We are excited to build on our extensive preclinical work with this hydrogel and get the technology ready to move into patients,” said Christman from the Jacobs School of Engineering at UC San Diego. The CIRM Translational Program provides key funds for moving this technology forward through what is traditionally the “valley of death” for many medical technologies.”
The team includes Dr. Ehtisham Mahmud, division chief of cardiovascular medicine, and medical director of the UC San Diego Sulpizio Cardiovascular Center, and Dr. Emerson C. Perin, medical director of the Stem Cell Center at the Texas Heart Institute.
“This is an extremely exciting development for the field and this project. The collaborative environment at UC San Diego has enabled us as bioengineers and cardiovascular interventionalists to translate this preclinical concept. Support from CIRM will enable us to perform product safety and dose finding studies to ultimately move forward with the pivotal clinical trial”, stated Mahmud, the study co-investigator.
The team had already shown that injection of a gel derived from cardiac muscle tissue extracted from pigs could help repair the heart after a heart attack. The tissue is stripped of cells, leaving behind a scaffold of the extracellular matrix from cardiac muscle, which acts a regenerative environment where cells can grow again. The cardiac hydrogel is currently being tested in a clinical trial in heart attack patients and is being developed by Ventrix, Inc., a startup cofounded by Christman.
Using this same concept, Christman and her team developed a material that was derived from the skeletal muscle of pigs to treat damaged skeletal muscle. Researchers injected the gel into the affected area in a rat model of peripheral artery disease seven days post-surgery and monitored blood flow in the rats’ limbs up to 35 days after injection.
Researchers found that the hydrogel increased the diameter of the rats’ larger blood vessels, called arterioles. The increased diameter led to improved blood flow in the limbs. By day 35, the size and structure of muscle fibers in the rats treated with the hydrogel was comparable to that in healthy rats.
The gel, which forms a fibrous scaffold upon injection, also attracted muscle stem cells to the affected area. Gene expression analysis showed that inflammatory response and cell death decreased while blood vessel and muscle development pathways increased in rats injected with the gel.
The team is now planning to perform additional preclinical safety tests to get ready for a first-in-man trial. They will also work with Ventrix, Inc. to manufacture clinical grade material.
The team received previous funding from the Heart, Lung and Blood Institute at the National Institutes of Health and the American Heart Association.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.


