
DELPHI Project Foretells Future of Personalized Population Health
NSF awards $2 million over four years to UC San Diego computer scientists and physicians
By:
- Doug Ramsey
Published Date
By:
- Doug Ramsey
Share This:
Article Content
Imagine a new type of healthcare app that does it all – it helps you understand your current health status, assists you in making changes in your life to improve your health, and takes into account the perspective of your entire life history, others in your age group--and perhaps even your neighborhood-- who share similar characteristics.
That’s the vision put forward by a team of physicians and computer scientists at the University of California, San Diego who are collaborating on a new digital resource that would take advantage of advances in databases, cyberinfrastructure and machine learning to usher in a new era of health and health care.
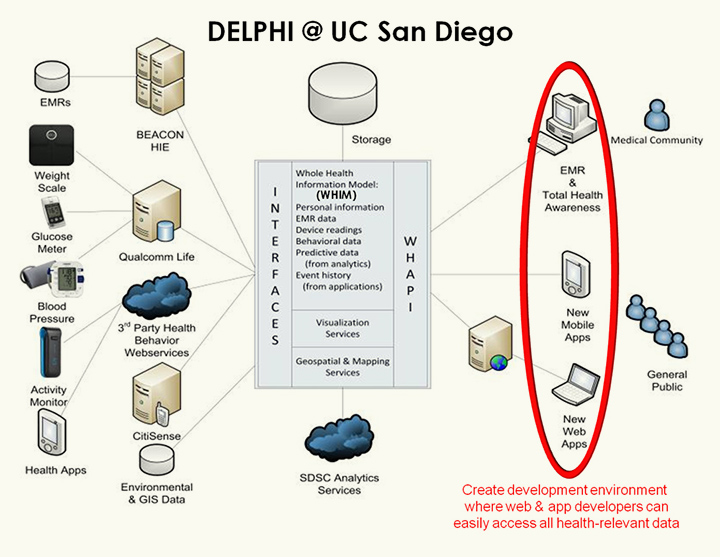
Structure of the DELPHI e-platform at UC San Diego
“Patients, providers and consumers need to be empowered by apps and services that leverage the full range of data that are essential to health promotion, disease prevention and medical care. We characterize this as personalized population health,” said Kevin Patrick, a professor of family and preventive medicine in the UC San Diego School of Medicine. “Opening up access to personal, medical, environmental and population-level data can enable designers and developers of the ever-increasing numbers of wearable health monitoring devices, smartphone apps, and web-based health to create new products and services that are truly tailored to the individual. These can do everything from spelling out ways to improve your health by adopting appropriate behaviors to where to go on a holiday weekend when you or a loved one have run out of a life-critical medication.”
The National Science Foundation (NSF) has awarded $2 million over four years to the UC San Diego team to prototype the development of a “Data E-platform Leveraged for Patient Empowerment and Population Health Improvement” (DELPHI).
“The acronym is particularly meaningful,” noted Patrick, principal investigator on the DELPHI project and director of the Center for Wireless and Population Health Systems in the California Institute for Telecommunications and Information Technology (Calit2). “If we get it right, this new platform can become a modern-day oracle – giving a glimpse into the present and the future of users based on an understanding of all health data that are known to influence both present health and risks to health over time.”
The DELPHI platform builds on existing projects and capabilities developed on the UC San Diego campus by the School of Medicine, the UCSD division of Calit2, the Jacobs School of Engineering’s Department of Computer Science and Engineering (CSE), and the San Diego Supercomputer Center (SDSC).
The project brings together a team of physicians (PI Kevin Patrick and co-PIs Theodore Chan, Lucila Ohno-Machado and Jeannie Huang) and CSE faculty (co-PIs Bill Griswold, Yannis Papakonstantinou and Sanjoy Dasgupta), who have collaborated on previous cyberinfrastructure projects, as well as SDSC’s Chaitan Baru. These projects include the CitiSense and CYCORE projects, which focused, respectively, on the real-time capture of environmental data for personal health, and collecting data from individuals at home in the context of clinical treatments. (CitiSense was funded by the National Science Foundation, and CYCORE by the National Institutes of Health.)
“Now imagine if you could federate all of the data silos, or islands, and get insights from piecing together data that appear in individual silos,” said co-PI Griswold, who leads the CitiSense project. “If you can then put a machine-learning and ‘Big Data’ analytics layer on top of it, DELPHI would start to fulfill the promise of personalized population health.”
Community partners will play a central role in the project. In addition to Qualcomm Life and its 2Net Hub & Platform infrastructure, the partners include the County of San Diego Health and Human Services Agency, San Diego Association of Governments, CONNECT, and San Diego Beacon Community. The latter is a partnership of health care providers, clinics, hospitals, emergency medical services and public health organizations that has invested in a health information exchange (HIE), an electronic network that allows San Diego health care providers to access patient health information from different electronic-record platforms and health care sites.
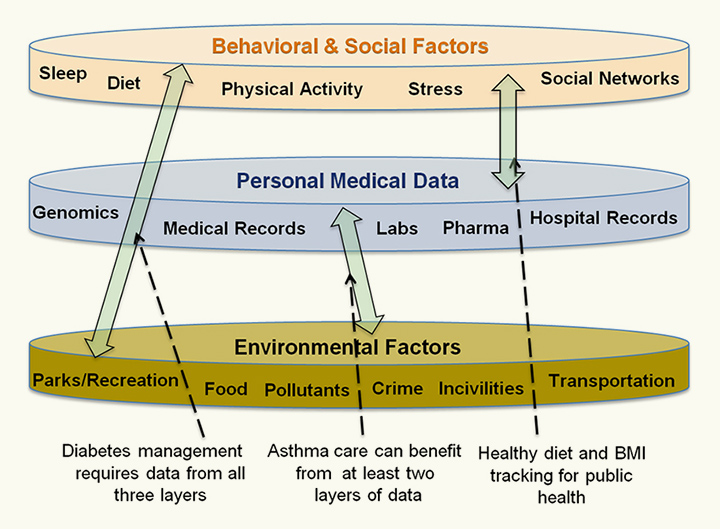
The DELPHI resource will allow apps designers to integrate real-time, population-scale health data from the personal, behavioral and social as well as environmental spheres in order to put the individual in the broadest possible context -- and to improve care such as diabetes management, which requires information from all three layers of data.
“The San Diego Beacon Community is one of the best models in the nation of how local regions can develop new methods of sharing medical record data to improve the delivery of health care services to the population at large,” said Dr. Chan, who founded the Beacon Community initiative in 2010 with support from a grant from the U.S. Department of Health and Human Services.
Another important part of DELPHI is how it supports convergence among key components of the new ecosystem of health and healthcare. Software developers have created thousands of health care apps for iPhone and Android devices, while others involved on the hardware side are creating a variety of new wearable and home-based technologies that provide 24/7 collection of data on a person’s vital signs, diet, activity, weight and other metrics of personal health.
“Despite the endless streams of personal data that these apps and technologies provide, they are still relatively modest in terms of their impact on health,” said co-PI Griswold. “One-of-a-kind wearable devices or apps like Nike+, Calorie King, or Zeo (for sleep) that utilize computer or Web-based platforms have basically zero ability to interchange data with electronic medical records, reducing their utility for individuals and their health care providers.”
The data from such apps also do not correlate to other personal medical data, including a patient’s genomic information, prescription drug use, or hospital records. Nor do they do anything at all with the capabilities that we now have to use cloud computing and real-time analytics to provide comparative data on other people based on age, education, geophysical location or other parameters. The vision of DELPHI is to set the stage such that data from these personal devices can intersect with data from two other layers (see graphic) of important information: electronic medical record data on genomic, biologic, and physiological data; and data on environmental factors important to health such as air pollutants or resources that promote higher levels of physical activity or stress reduction.
“Management of most health problems requires data from more than one of these layers for effective prevention or treatment,” noted Patrick. Diabetes management, for example, leverages information from all three layers because it involves a combination of careful tracking of insulin dosing blood glucose, promoting physical activity and diet behaviors through evidence-based approaches for behavioral improvement, and an understanding the home, neighborhood, social and community context of the patient.
“We too often just assume that if we address one of these issues we’ve solved the problem” says Patrick. “This is what is so often frustrating to patients as they see their doctors managing the numbers related to their illness, but ignoring the larger context of what actually influences their lives. The vision of DELPHI is that we can open up all of these data so that health services can be provided in a more holistic and complete way.”

'Health 3.0' is the vision of DELPHI researchers for personalized population health apps for Web, desktop and mobile devices.
It is a tall order to bring all of this information together through a single resource, but that is the goal of DELPHI’s integrated “whole health information model,” which Griswold dubbed “Health 3.0”, going beyond today’s Web 2.0 health apps. Consumers, patients and software developers would then be given access to the digital database to monitor their own health – or to create a whole new generation of apps and services that will go well beyond charting a person’s heart rate or blood oxygen levels.
Advances in database technologies, integrating and using very different forms of data are necessary to deal with the tremendous volume and real-time nature of the data, and DELPHI researchers hope to use machine learning to handle the variety of data that will be spread across disparate stakeholder platforms.
“We need to provide integrated access and analysis of all data relevant to health,” said co-PI and computer science professor Yannis Papakonstantinou. “This means that we need to make it easier to draw inferences from the ‘noisy’ data – some of it semi-structured, some streaming, and all of it distributed across diverse stakeholder platforms.” Moreover, according to Sanjoy Dasgupta, an expert in machine learning and also a co-PI on the project, “The DELPHI platform has to enable novel forms of analyses based on contextual and statistical metadata.”
DELPHI would make it possible for a wide community of software and hardware developers – from full-time professionals to relative novices – to program apps or develop services on top of a real-time, population-scale health and medical dataset. This is the rationale behind engaging UCSD CONNECT in this project. With an internationally recognized track record of connecting entrepreneurs to scientists of all types, DELPHI hopes to leverage the relationships that CONNECT has in the startup, developer and venture funding communities to help focus new developments on this ‘whole health information model.’
“If we are successful, there will be less fragmentation and Balkanization in new tools and services, and more harmonization of products and services that actually work together to promote personalized population health,” concluded principal investigator Kevin Patrick. “By analyzing new database and machine learning techniques in realistic field trials, we hope to arrive at new insights on the nature of computing for health and medicine in a world of big data – and even bigger health challenges for us all.”
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.


