
By:
- Scott LaFee
Published Date
By:
- Scott LaFee
Share This:
Minding Time: Department of Psychiatry Marks 50 Years
Nineteen-hundred-and-sixty-nine was a famously memorable year. It was the year of Woodstock and the first man on the moon, of the Cuyahoga River in Cleveland catching fire and the last public performance by The Beatles—an impromptu concert atop Apple Records in London.
It was the debut of The Brady Bunch and square hamburgers from a new restaurant called Wendy’s. The University of California San Diego wasn’t yet even a teen; the School of Medicine was even younger, founded just one year earlier.
Nineteen-hundred-and-sixty-nine also marked the beginning of the School of Medicine’s Department of Psychiatry. This year marks its 50th anniversary.
From the beginning, the department was different, and equally memorable. Its founding chair was Arnold J. Mandell, M.D., a 35-year-old neuroscientist and psychiatrist who was, at the time, the youngest physician ever appointed chair of a medical school psychiatry program in the United States.
Mandell was an early advocate of biological psychiatry, the concept that mental disorders could be studied and understood in terms of the underlying biological functions of the brain and nervous system. The approach encompasses multiple disciplines: neuroscience, psychopharmacology, biochemistry, genetics, epigenetics, physiology and more. It moved beyond the older practices of exploring a patient’s state-of-mind through talk, dreams, free association and fantasies.
As a result, the Department of Psychiatry at UC San Diego School of Medicine became the first in the country with a biological orientation, an approach emphasizing the requirements and values of empirical science.
Mandell stepped down as chair in 1977 and later moved to the Cielo Institute, a North Carolina-based center for biophysical theory and applications, though he retains professor emeritus status at UC San Diego.
He was succeeded by one of his first recruits, Lewis Judd, M.D. Like Mandell, Judd was a forceful expert in biological psychiatry, particularly regarding the idea that mental disorders like depression could be treated with appropriate, rigorously developed psychopharmaceuticals.
Judd devoted the rest of his career to building one of the country’s finest psychiatry departments, based on research and evidence, elevating it to among the top three in National Institutes of Health funding. From 1987 to 1990, he served as director of the National Institute of Mental Health, the first active scientist to hold the job and helped launch the Decade of the Brain (1990-1999), an ambitious effort to raise public awareness of the benefits derived from brain research.
“The thing I’m most proud of is how psychiatry is becoming increasingly recognized as a real biomedical science,” Judd said in 2013. “It used to be disdained. A broken mind wasn’t as real as a broken bone. We lionized physical medicine, but dismissed brain biology, which has an enormous effect upon not just our behavior, but our bodies as well.”
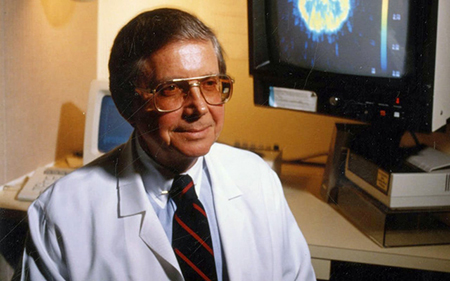
Lewis Judd, MD. U.S. National Library of Medicine
Judd retired in 2013 after 36 years as chair, serving an astounding 70 percent of the university’s existence at the time. He died in 2018 at the age of 88.
Igor Grant, M.D., became only the third chair of psychiatry in 2014. Grant, who joined UC San Diego faculty in 1972, embodies the department’s extraordinary scope and depth of research. He is director of the HIV Neurobehavioral Research Program, which includes the California NeuroAIDS Tissue Network, the Translational Methamphetamine AIDS Research Center, the HIV Neurobehavioral Research Center and the CNS HIV Anti-Retroviral Therapy Effects Research.
Under Grant, the department has seen a period of significant growth and change, most notably in the focus and expansion of the clinical enterprise, with significant advances in UC San Diego Health programs and quality, including patient access, satisfaction and experience.
Several academic initiatives have also been launched, including a collaboration with UC San Diego’s Jacobs School of Engineering to begin developing a Mental Health Technology Center. Recent years have also witnessed new faculty recruitments in basic and translational science, as well as expansion of multidisciplinary training.
“Fifty years ago, we were among the groundbreakers in the idea that the brain had to be put back into psychiatry,” said Grant. “As we and others have embraced this paradigmatic shift, we have come to understand that alterations in mood, behavior and cognition are not simply the product of something being ‘wrong’ structurally with the brain. Behavioral disturbances can reflect altered patterns of communication between distributed neural networks. Connectivity among circuits may be overly strong, too weak or asynchronous.
“We now view the brain as a constantly adapting system. Nature and nurture are not separate universes, but in constant interplay. We come into the world with certain endowments, and these exert some limits on what we think and do, but the brain is a system that constantly learns, creates behaviors and those behaviors and learning continue to reprogram it, including at a genetic level."
Igor Grant, MD.
In addition to impactful research, the department’s mission includes training and preparing mental health professionals for the future. The earliest programs focused on training psychiatrists, emphasizing evidence-based practices. In the 1980s, efforts expanded to train psychologists in the scientist-practitioner model, partnering with San Diego State University. Over the years, this top-ranked doctoral program has grown to encompass 25 distinct multidisciplinary specialties, including clinical and research training in addictions, child psychiatry, geriatric psychiatry, HIV/AIDS, eating disorders, neuropsychology, and biological psychiatry.
Grant said the future of psychiatry—or at least the vision at UC San Diego—likely involves developing new technologies to alter ingrained patterns of neural communications—strengthening where needed, weakening elsewhere.
“We are developing strategies to understand how communications within and between cells are altered in psychopathological states. We propose to use techniques developed with our engineers first to monitor these communication patterns between circuits in real time, to identify targets of intervention and then evaluate the effects of interventions.
“These interventions need not be limited to drugs or electromagnetic brain stimulation. Indeed, one of the exciting challenges will be to determine and monitor how verbal and nonverbal communications can be optimized to modify the brain’s responses in predictable ways. I expect this great department to contribute to improved mental health outcomes in the decades to come.”
For the full version of this story, click here.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.


