
By:
- Scott LaFee
Published Date
By:
- Scott LaFee
Share This:
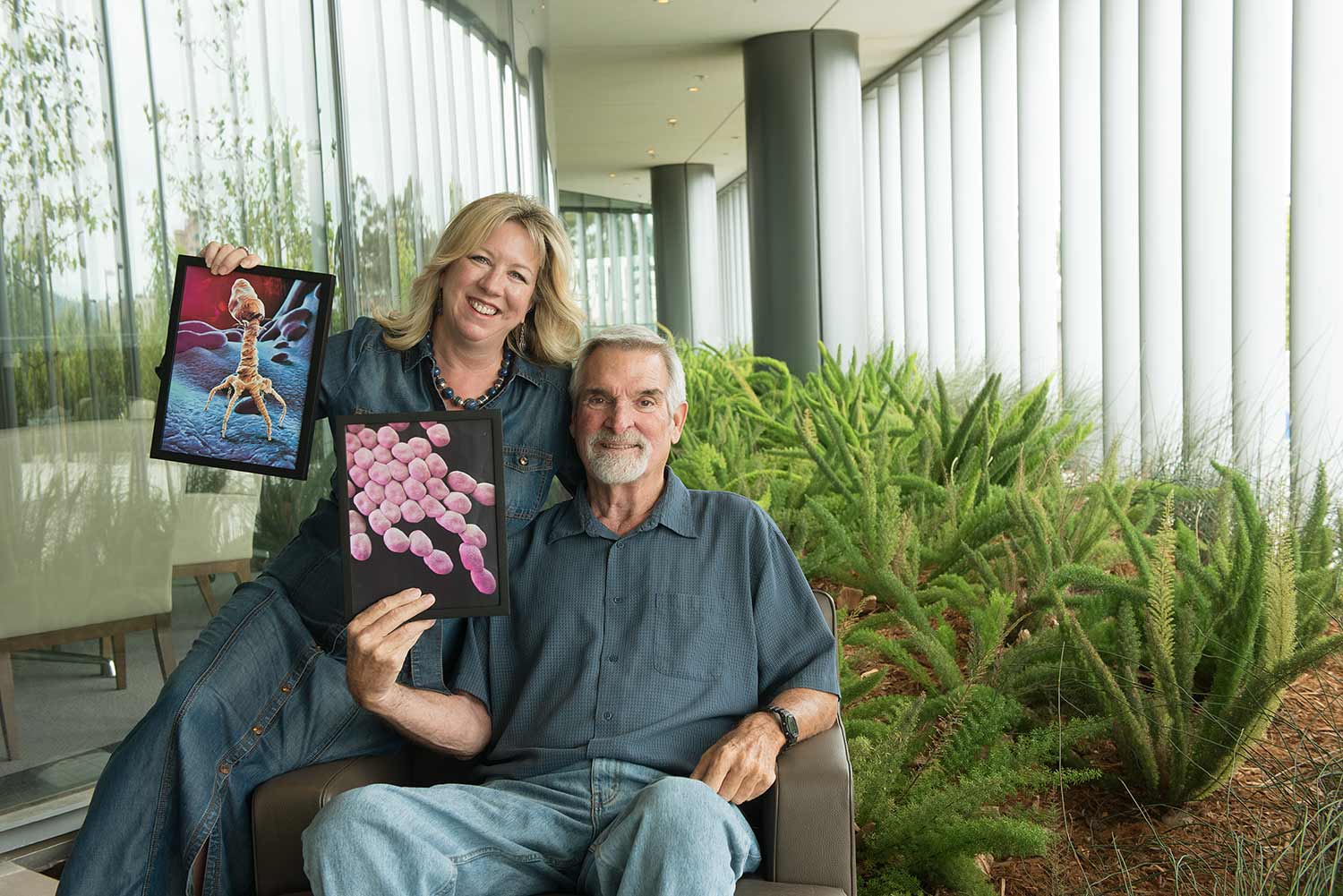
Steffanie Strathdee holds an image of a bacteriophage; her husband, Tom Patterson holds a rendering of A. baumannii, the bacteria that almost killed him.
TIME’s List of 50 Most Influential People in Health Care Includes a Real ‘Phage’ Turner
Medical drama propelled UC San Diego epidemiologist to forefront in fight against multidrug-resistant bacteria
In the beginning—and near the end—Steffanie Strathdee’s only goal was to save her husband’s life. In 2016, Tom Patterson lay unresponsive in a coma at the Thornton Intensive Care Unit, part of the Jacobs Medical Center at UC San Diego Health. He was stricken by a multidrug-resistant bacteria that had systemically overwhelmed his body, defying all modern antibiotic treatment.
Patterson was dying.
But Strathdee, an epidemiologist and associate dean of global health sciences at UC San Diego School of Medicine, would not give up hope. She had read about bacteriophages—viruses that specifically target bacteria, their name meaning “bacteria eaters—and she urged her colleagues in the School of Medicine to try them.
It would be a first as a last resort.
“To our knowledge, Tom was the first patient in the United States with an overwhelming, systemic infection to be treated with this approach using intravenous bacteriophages,” said Dr. Robert “Chip” Schooley, who pursued the unprecedented therapy. It would require emergency approval from the Food and Drug Administration and hurried coordination among multiple institutions, physicians and scientists across the country.
It worked. Patterson awoke from his coma and, over the next several months, fully recovered and returned to his position as a professor in the Department of Psychiatry in the School of Medicine.
Since Patterson’s unprecedented treatment, five more patients at UC San Diego Health have been treated with phages, including a patient this year with a years-long chronic infection that was successfully cleared, allowing him to undergo life-saving heart transplant surgery. In all cases, the phage treatments were considered experimental and required emergency approval by the FDA.
Last week, Strathdee was named one of TIME magazine’s inaugural 50 Most Influential People in Health Care for 2018, which identifies people who “have changed the state of health care in America this year, and bear watching for what they do next.”
“It’s a great honor to be recognized for my efforts to bring phage therapy into the 21st century in North America,” said Strathdee, “but it all started with my single-minded desire to save my husband’s life, and it truly reflects a team effort.”
Indeed. In June, UC San Diego School of Medicine announced creation of the interdisciplinary Center for Innovative Phage Applications and Therapeutics (IPATH), funded by a three-year, $1.2 million grant from UC San Diego Chancellor Pradeep Khosla. IPATH is the first such center in North America. It is co-directed by Strathdee and Schooley, who is also senior director for international initiatives in the UC San Diego Office of International Affairs.
“The story of how phages saved Tom’s life and have helped others, the tremendous depth of scientific knowledge and medical practice, combined with intuition, innovation and just sheer guts, is what UC San Diego is all about,” said Khosla, announcing the grant. “IPATH captures many of our most cherished ambitions: a robust, interdisciplinary research that advances science, but also delivers tangible benefits to patients and society. Phage therapy has the potential to save millions of lives.”
Bacteriophages are ubiquitous viruses, found wherever bacteria exist. Each viral species targets a specific strain of bacteria. Successful treatment requires finding the precise combination of phages to attack and eliminate a specific bacterial infection. Patterson was infected by a multidrug-resistant strain of Acinetobacter baumannii, an opportunistic pathogen that tops the World Health Organization’s list of the 12 deadliest multi-drug resistant bacteria. With rapid assistance from the U.S. Navy, FDA, Texas A&M University, San Diego State University and Ampliphi BioSciences, a San Diego-based biotech, Patterson was treated with a highly refined cocktail of phages originally derived from sewage.
Though investigated as a potential treatment for infections in the early 20th century, phage therapy was broadly discarded with the advent of antibiotics. Patterson’s case—and a handful of others in the United States and elsewhere—have reinvigorated interest in the approach, particularly given the growing, global threat of antibiotic resistant superbugs.
Strathdee, who holds the Harold Simon chair in the Department of Medicine, has been central to that effort. She began taking calls from patients around the world infected by multidrug-resistant bacteria, all desperate for treatment. Strathdee gave a TEDx talk on the subject and, with Tom, wrote a book called “The Perfect Predator,” slated to publish next year. Schooley, Patterson and Strathdee gave the closing plenary speech at this month’s IDWeek in San Francisco. She even got a nickname on Twitter: Superbug Slayer.
To be sure, phage therapy hasn’t quite slayed anything yet. Bacteria and phages have been doing an evolutionary dance since life began on Earth. It will continue, but perhaps with a nudge here and there from researchers like Strathdee and her colleagues.
In recent months, IPATH researchers have consulted with dozens of patients and outside medical teams to determine whether patients were good candidates for phage therapy. Roughly half, said Schooley, qualified, with a smaller number ultimately treated elsewhere.
“IPATH builds upon what we’ve learned and will apply rigorous principles that span from bench to bedside to better understand the potential role for phage therapeutics in the treatment of patients with infections that cannot successfully be treated with currently available antibiotics,” said Strathdee.
“It taps into and enhances a wide range of existing clinical and translational research programs and fosters emerging collaborations with the U.S. Navy Medical Research Center, industry partners and the strengths of the UC San Diego Health system.”
“Tom’s saga—and the incredible efforts of UC San Diego Health doctors and scientists—was a real-life medical drama,” said Dr. David Brenner, vice chancellor of health sciences at UC San Diego. “There are few places in the world with the resources, talented people and collaborative spirit required to do what was done here, to save a man’s life when every other tool of modern medicine was failing.
“We celebrate Steffanie’s achievement and honor all of the physicians, nurses, researchers and staff at UC San Diego Health and elsewhere who made this a story of recovery, hope and the future.”
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.


