Harnessing Cancer’s Methylation Footprint for More Precise Diagnosis and Prognosis
A bit of basic genetic machinery could help identify malignant tumors more easily and with greater accuracy
Published Date
By:
- Scott LaFee
Share This:
Article Content
In a new study, published online in the July 26 issue of PNAS, researchers at University of California San Diego School of Medicine, with colleagues in Xijing Hospital and Sun Yat-sen Cancer Center in China, report that DNA methylation can provide effective markers for at least four major cancers, not only correctly differentiating malignant tissues from normal, but also providing information on prognosis and survival.
“Choosing the proper cancer treatment with the best chance of recovery and survival depends greatly upon accurately diagnosing the specific type or subtype of cancer,” said Kang Zhang, MD, PhD, founding director of the Institute for Genomic Medicine and co-director of biomaterials and tissue engineering at the Institute of Engineering in Medicine, both at UC San Diego School of Medicine. “If you can do that using a minimally invasive biopsy, it has significant implications for cancer science and medicine. Using DNA methylation markers may be a new and more effective a way forward.”
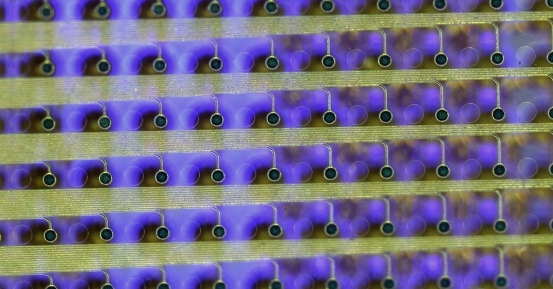
DNA methylation involves methyl groups — one carbon atom bonded to three hydrogen atoms — attaching to DNA molecules. It is a fundamental epigenetic process that regulates gene function without changing the DNA sequence of a gene, essential to normal development and associated with numerous key processes, including initiation and progression of cancer.
Zhang and colleagues looked at DNA methylation for differentiating tumor tissue and normal tissue for the four most common cancers (lung, breast, colon and liver) in three different databases: a training cohort of 1,619 tumor samples and 173 matched adjacent normal tissue samples; a testing cohort of 791 tumor samples from The Cancer Genome Atlas and 93 matched adjacent normal tissue samples and another independent testing Chinese cohort of 394 tumor samples; and 324 matched adjacent normal tissue samples.
They found that DNA methylation analysis could predict cancer versus normal tissue with more than 95 percent accuracy in the three cohorts, comparable to typical diagnostic methods, according to Zhang.
In addition, the analysis correctly identified 97 percent colorectal cancer metastases to the liver and 94 percent colorectal cancer metastases to the lung. “Since 10 percent of cancers present as metastatic lesions or cancers of unknown primary origin, identification of tissue of origin is critical for choosing a correct therapy. This new simple method will be of great value to pinpoint the primary source of the tumor,” said Michael Karin, PhD, co-senior author of the study and Distinguished Professor of Pharmacology, also at UC San Diego School of Medicine.
Zhang suggested DNA methylation has the potential to improve outcomes by providing more accurate diagnoses, particularly of relatively indolent or aggressive tumors that may require more or less aggressive treatment.
“Although we focused on just four common cancers here, we expect that DNA methylation analysis could be easily expanded to aid diagnoses of a much larger number of cancers,” said Zhang. “A great benefit is that this approach requires only a small amount of tissue to obtain adequate DNA for analysis, potentially allowing the use of less invasive biopsies or biopsies of metastatic lesions where the tumor is of unknown primary cancer type.”
He said more studies have been planned to fully explore the clinical applications and potential of DNA methylation and its role in future personalized cancer care.
Co-authors include: Xiaoke Hao, Fourth Military Medical University, Xi’an, China; Huiyan Luo and Rui-hua Xu, Sun Yat-sen University Cancer Center, Guangzhou, China; Michal Krawczyk, Wei Wei, Ken Flagg, Jiayi Hou, Shaohua Yi, Maryam Jafari, Danni Lin, Christopher Chung, Bennett A. Caughey, William Shi, Jie Zhu, Xin Fu, Edward Zhang, Charlotte Zhang, and Debanjan Dhar, UC San Diego; Heng Zhang, Lianghong Zheng, and Rui Hou, Chinese Academy of Sciences, Shanghai, China; and Gen Li and Liang Zhao, Guangzhou Youze Biological Pharmaceutical Technology Company, Guangzhou, China.
Funding for this research came, in part, from the Carol and Dick Hertzberg Fund, the Richard Annesser Fund and the Michael Martin Fund.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.