Underlying Molecular Networks Suggest New Targets to Combat Brain Cancer
SDSC/UCSD team uncovers signaling links to glioblastoma factor
Published Date
By:
- Warren Froelich
Share This:
Article Content

Glioblastoma is a highly aggressive form of brain cancer with a survival rate generally less than 16 months. With no effective treatments available, a team including researchers from the San Diego Supercomputer Center (SDSC) at UC San Diego and John Wayne Cancer Institute at Providence Saint John’s Health Center sought to uncover several underlying molecular networks that may yield attractive therapeutic targets for this deadly disease.
The results, published in the July 16 online issue of Oncotarget, focus on a transcription factor called OLIG2 (Oligodendrocyte lineage transcription factor), known to play a critical role in brain tumor development. Transcription factors control which genes are turned “on” or “off” at any given time.
“This study offers a new way of thinking about, and establishing priorities for, treatment options for glioblastoma,” said first author Igor Tsigelny, a research scientist with SDSC as well as at the UC San Diego Moores Cancer Center and the university’s Department of Neurosciences.
Specifically, the team created a series of molecular networks or “modules”, grouping together genes related to OLIG2. Among other things, the researchers found that molecules in each module tended to organize themselves according to specific functions in various processes related to cancer: some turn cell functions on and off; others direct cell proliferation and differentiation; others signal the formation of blood vessels to tumors; and so on.
“The results suggest that drug development efforts should be looked at from the perspective of signaling networks including critical hubs and identifying combination therapies to overcome resistance mechanisms,” said Santosh Kesari, the study’s senior author and the Chair of Translational Neuro-Oncology and Neurotherapeutics at the John Wayne Cancer Institute and the Pacific Neuroscience Institute, both located in Santa Monica.
Like many cancer-forming genes, OLIG2 initially plays a role in the growth and function of “normal” cells and tissues, in this case working during specific developmental stages to create neural stem cells that form the central nervous system. This function of OLIG2 is subsequently shut down once its mission has been completed. But with brain cancer, there’s significant evidence that OLIG2 is switched back “on”, promoting the activity of cell growth and survival genes when they should not be, leading to fast-growing tumors.
Given this evidence, the researchers decided to identify OLIG2-related signaling pathways and genes responsible for its activity, using a systems biology approach to build a “hierarchical” gene network based on their relationships to other molecules. Genes with the largest number of interconnections or relationships were placed at the top of the hierarchy, with others having fewer connections falling underneath.
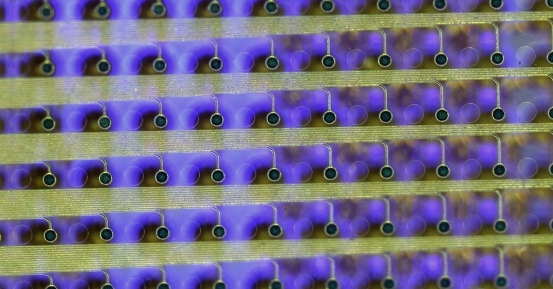
To create their network, the researchers -- who included Valentina Kouznetsova, associate project scientist at SDSC and UC San Diego; and Nathan Lian, a student in the Research Experience for High School Students (REHS) summer program at SDSC -- turned to a computer program called VisANT, a web-based tool for mining data, used for biological pathway analysis and for querying the visualization of gene regulation and gene networks for glioblastoma. In addition to simple networks, interactions in VisANT also were used to define high-level connections between groups of proteins, complexes, pathways, sub-networks, or simply “gene modules.”
“Essentially, VisANT has an intrinsic database of functional links between proteins. It helps to show a comprehensive picture of numerous interactions between all available genes in the gene network, grouping them based on connectivity with surrounding genes,” said Tsigelny.
“Because genes in these modules are working together and the modules are hierarchically integrated in biological networks, we call them coherent-gene modules (CGM),” added Kesari.
After further refinement of genetic signaling networks with other software, the results showed that families of molecules interacting with OLIG2 in brain cancer form eight CGMs.
Aside from observing how molecules in each module tended to organize themselves according to specific functions in various processes related to cancer, the modules revealed “feedback loops” in signaling pathways involving OLIG2 that create conditions for the constant activation of proteins responsible for tumor growth and its rapid spread.
“Receptors included in these loops activate the most notorious carcinogenic pathways,” said Kesari.
In addition, the research identified the gene in the hierarchy with the most connections as epidermal growth factor receptor (EGFR); followed by HSP90, which stabilizes the number of proteins required for tumor growth, and CALM1, regulators of cell signaling and neurotransmitter function; and then KDM1A and NCOR1, both epigenetic factors.
“There are treatments of EGFR overactivation,” Tsigelny said. “The KDM1A and NCOR1 are involved in epigenetic regulation and their activation has to be also addressed. So, the bottom line is that a drug combination has to take into account both.”
This latest research relates to a previous study published last year in which Valentina Kouznetsova and coauthors developed a computational strategy to search databases for 3D molecular structures for small molecules that might engage a hotspot between OLIG2 and partner proteins. With this approach, Tsigelny and Kesari identified a few molecules that would likely fit the OLIG2 interaction, and then tested a few for their ability to kill glioblastoma tumors.
“The current research suggests that the “positive feedback loops” have to be interrupted with specific combinations of drugs, rather than a single therapeutic agent directed against one specific activity or pathway,” said Kesari.
Grants from American Brain Tumor Association Drug Discovery Grant (in tribute to Francis X. Colden III), and Voices Against Brain Cancer to S. Kesari provided support for this research, in addition to the Chemical Computing Group and Chris Williams.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.