Breastfeeding May Protect Infants from HIV Transmission
Compound in human milk associated with reduced transmission from HIV-infected mother to breastfed infant
By:
- Debra Kain
Published Date
By:
- Debra Kain
Share This:
Article Content
An international team of researchers has found that certain bioactive components found in human milk are associated with a reduced risk of HIV transmission from an HIV infected mother to her breast-fed infant. Their study will be published in the August 15 online edition of American Journal of Clinical Nutrition.
“In developing countries, HIV-infected mothers are faced with the decision of whether or not to breastfeed their babies,” said Lars Bode, PhD, assistant professor in the Department of Pediatrics at the University of California, San Diego School of Medicine. “Breastfeeding exposes the baby to the virus and increases the risk of the baby dying from HIV infection; but not breastfeeding increases the risk for the baby to die from other intestinal or respiratory infections.”
Bode and colleagues set out to find why the vast majority of breast-fed infants do not acquire HIV-1, despite continuous exposure to the virus in their mother’s milk over many months. Even in the absences of antiretroviral drugs, only 10 to15 percent of infants will acquire HIV infection from their HIV-infected mothers.
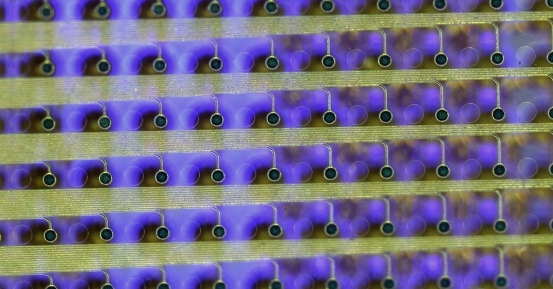
They discovered that immunologically active components called human milk oligosaccharides (HMO) – a type of carbohydrate made up of several simple sugars linked together – may protect from HIV transmission. These complex oligosaccharides are the third-most abundant component of breast milk, yet are not digestible and therefore become highly concentrated in the mucosal surfaces of the infant’s gastrointestinal tract.
“HMO act as prebiotics that promote the growth of desirable bacterial communities in the infant’s intestine,” said Bode. Additionally, HMO structurally resembles sugar chains called glycans that are normally found on epithelial cell surfaces, and can serve as “decoy” receptors to inhibit pathogens from binding. Last, HMO exhibit anti-inflammatory activity and have been shown to modulate immune cell responses in cell and animal models.
The researchers analyzed HMO amount and composition in breast milk samples collected from more than 200 women as part of a larger study of HIV-infected women and their infants in Lusaka, Zambia, following them from birth to 24 months. (Most were recruited to the study and followed before antiretroviral therapy became available to them, thus offering a unique look at associations between HMO and HIV transmission.)
Higher concentrations of HMO in milk were associated with protection against postnatal HIV transmission, independent of other known risk factors. In the future, a better understanding of how individual HMO facilitate or obstruct HIV transmission may guide the development of interventions to complement antiretroviral strategies and more effectively prevent transmission, according to the researchers.
Additional contributors to the study included Lauren Hsiao and Caroline Nissan, UC San Diego; Louise Kuhn and Hae-Young Kim, Columbia University; Moses Sinkala, Lusaka District Health Management Team, Zambia; Chipepo Kankasa and Mwiya Mwiya, University Teaching Hospital, University of Zambia; Donald M. Thea, Boston University; and Grace M. Aldrovandi, Children’s Hospital Los Angeles, USC.
Funding was provided by the National Institute of Dental and Craniofacial Research (NIDCR) (DE021238) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), National Institutes of Health (NIH) (HD39611, HD40777, HD57617) and a University of California, San Diego, Center for AIDS Research Pilot Development Grant.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.