
New Technology is Life-Saving Voice for Premature or Critically Ill Infants
Innovative monitoring system detects risk of infections up to 24 hours before symptoms appear
Published Date
By:
- Michelle Brubaker
Share This:
Article Content

Melissa Renteria holds her newborn baby, Arthur, while he’s monitored by the HeRO technology.
A new technology in the Neonatal Intensive Care Unit (NICU) at UC San Diego Health is able to predict the risk of life-threatening infections up to 24 hours before they appear in severely premature or critically ill infants. Infection is the leading cause of death in this fragile patient population.
The Heart Rate Observation system, or HeRO, is an innovative monitoring technology that uses an algorithm to detect slight changes in a baby’s heartbeat that could be an early sign of a major infection, like sepsis — a bacterial infection that is highly dangerous to babies born three pounds or less.
“The challenge with diagnosing sepsis is a lot of symptoms for the early stages of the infection are subtle and nonspecific,” said Erika Fernandez, MD, director of the NICU at UC San Diego Health. “With the HeRO technology, we can detect symptoms of sepsis up to 24 hours before the infection actually happens. This allows us to begin an investigation and intervene with treatment before a baby becomes critically ill.”
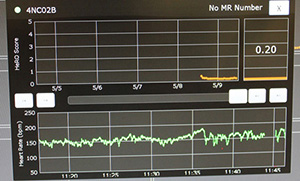
New technology monitors Arthur’s heart rate to detect signs of infection.
UC San Diego Health is the first health care provider in San Diego County to use the technology, which can detect infections in the blood stream and intestines. Historically, physicians and nurses have relied upon their own observations to detect signs of infection. The new system reports vital sign trends much earlier than the human eye or traditional equipment and requires no additional wiring to the baby.
“This state-of-the-art technology lets babies be babies, and mothers can breastfeed without worrying about tangling up or unplugging wires,” said Lawrence Prince, MD, PhD, chief in the Division of Neonatology at UC San Diego Health. “It makes for a much less intimidating experience for families and a highly improved monitoring approach for medical staff.
The HeRO system uses a zero-to-seven surveillance score generated after a heart rate is analyzed, with anything higher than a two considered an alert for possible infection. Prince says the technology is expected to reduce mortality rates in the NICU by 20 percent.
“Physicians and nurses can evaluate a situation much more thoroughly,” said Prince. “When I look at the data on the monitor, I can ask myself, ‘is there something more going on with the patient and do we need to do further testing?’”
Fernandez added that the monitoring system represents part of the next generation of technology to save lives and help achieve the ultimate goal in the NICU: “To provide the highest quality of comprehensive and compassionate care to NICU babies so they can thrive and go home with their families as soon as possible.”
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.


