Start-up Receives up to $15 M to Develop Nanoparticle Therapy for Sepsis Licensed from UC San Diego
Published Date
By:
- Liezel Labios
Share This:
Article Content
San Diego-based Cellics Therapeutics, which was co-founded by UC San Diego
CARB-X, which stands for Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator, is a global non-profit partnership dedicated to supporting early development of antibacterial R&D to address the rising threat of drug-resistant bacteria.
In a paper published in Proceedings of the National Academy of Sciences in
The CARB-X funds will go to Cellics and the Nizet Laboratory to develop an appropriate animal model for bacterial sepsis to carefully assess the therapeutic potential of the nanosponges. Researchers will also identify the appropriate cell line to be used for manufacturing the nanosponges. The ultimate goal is to advance Cellics’ manufacturing capabilities and scale up production of the
“Cellics is dedicated to the development of biomimetic nanomedicines to treat life threatening diseases. Our macrophage nanosponge technology leverages the natural receptors on human macrophage membranes to neutralize bacterial pore-forming toxins, endotoxins, and inflammatory cytokines that underlie sepsis,” said Dr. Steve Chen, president and chief medical officer, Cellics Therapeutics, Inc.
“Sepsis is a leading cause of death around the world that is made worse by the lack of effective preventatives and treatments for drug-resistant bacterial infections. Effective treatments are urgently needed,” said Erin Duffy, CARB-X R&D Chief. “CARB-X funds and supports early development of innovative antibiotics and other treatments that target the most dangerous drug-resistant bacteria. Cellics’ nanosponge product, if successful, could potentially transform the treatment of sepsis and save lives.”
Sepsis
Sepsis occurs when the body launches an uncontrolled immune response to an infection, triggering widespread inflammation that can lead to organ failure, septic shock and even death. The U.S. Centers for Disease Control and Prevention estimate that more than 1.5 million Americans get sepsis and about 250,000 die from this condition each year. A 2020 study in the leading medical journal The Lancet estimated that sepsis-related deaths represent 19.7% of all global deaths, exceeding cancer as a cause of human mortality.
Sepsis is usually treated with antibiotics. But while antibiotics can potentially eliminate sepsis-causing bacteria, they can’t keep inflammation in check.
Inflammation is triggered when macrophages recognize
Most recently, cytokine storm has emerged as a major issue in COVID-19, leading to organ injury and failure, and ultimately, if left unchecked, to death.
There is no currently approved treatment for sepsis. “To effectively manage sepsis, you need to manage this cytokine storm,” said Zhang.
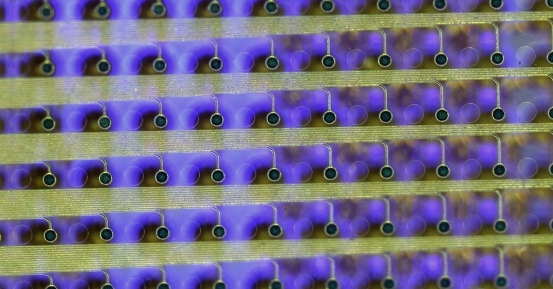
Nanosponges stop the cascade that leads to sepsis by trapping endotoxins and pro-inflammatory cytokines onto their macrophage cell membranes, thus neutralizing them. The injected nanosponges vastly outnumber the organism’s own macrophages, ensuring that sepsis and a cytokine storm can be avoided. Also, since the nanosponges are covered in actual macrophage cell membranes, they can pass as the body’s own immune cells and circulate within the bloodstream without being evicted.
The nanosponge platform
Sepsis-fighting nanosponges are one example of the cell membrane cloaking technology pioneered by Zhang’s lab at UC San Diego. His group develops new nanomedicine therapies by disguising nanoparticles as the body’s own cells. Previous examples include red blood cell nanosponges to combat and prevent MRSA infections; nanoparticles cloaked in platelet cell membranes to repair wounded blood vessels; and
In 2014, Zhang co-founded Cellics to further develop and commercialize th
Product development
The mission of Cellics is to employ innovative biomimetic nanomedicines to address serious diseases with a high unmet medical need. The
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.